Choosing A Career In Respiratory Therapy Has Brought Ismael Torres Adventure And Constant Learning
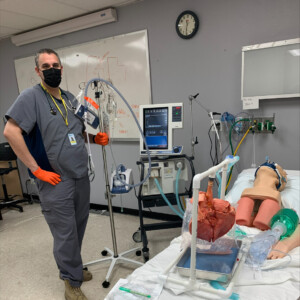
 Choosing a career in Respiratory Therapy (RT) has brought Ismael Torres adventure, constant learning, and what he describes as “the best job I’ve ever had.”
Choosing a career in Respiratory Therapy (RT) has brought Ismael Torres adventure, constant learning, and what he describes as “the best job I’ve ever had.”
Ismael grew up in Southern California and worked in a variety of odd jobs before choosing to attend the Respiratory Care program at Carrington College in Las Vegas, Nevada. That’s where he graduated in 2015 and did his clinicals at a nearby Long-Term Acute Care (LTAC) ward. His patients there were stable but generally needed multiple months to fully recover. He said that some of the patients were recovering from traumatic brain injuries and wouldn’t show progress for three to four months or even longer, while others were recovering from medical crises like heart attacks with respiratory-related issues that responded more quickly. This position taught him a lot and was a great launching pad for his career.
After working in the LTAC in Las Vegas, Ismael went into the adult and pediatric Intensive Care Units (ICU) at Renown Regional Medical Center in Reno for 4 years. At Renown, he also had the opportunity to step into their Level II trauma center where he expanded his knowledge and experience immensely. When asked if he was nervous about working in the trauma center, he said, “The great teacher I had at Carrington helped prepare me for stepping into that role.”
In 2019, Ismael was up for an adventure and he knew that the high demand for RTs afforded him the freedom to spend some time traveling and working in other places. So, he spent some time in Kansas City, Missouri, and returned to Las Vegas for a while. “I thoroughly enjoyed that experience—it was so much fun,” he said about his time traveling and working.
Then in February 2020, he was ready to return to Reno and work in nearby Carson City at Carson Tahoe Hospital in their ICU. The COVID-19 pandemic would soon follow. Treating COVID-19 patients has been challenging and frustrating for Ismael because “It is impossible to get ahead of COVID. Our usual practices and what we learn in school just doesn’t seem to work for patients with this disease.”
To Ismael’s relief, mask-wearing and social distancing practices were helping and COVID-19 cases slowed down briefly in his ICU. However, the State of Nevada just reported record positive test numbers and the ICU is full yet again. Ismael attributes this to citizens relaxing distancing and mask-wearing precautions, which he compared to patients not completing their prescription for antibiotics when they have an infection because they feel better—only to have their infection come roaring back again.
“Patients are told, ‘take this medicine until the bottle is empty’ and so they take it, but then as soon as they start feeling better, they stop taking it. That is exactly what is happening right now with COVID. The numbers got a little better, people backed off with wearing masks and taking precautions, and then the first wave of the virus, which seemed like it was starting to back off a little bit, resurged.”
Another cruel thing about COVID-19 is how it is disproportionately affecting minorities, especially the Hispanic and American Indian communities in the Sunbelt where Ismael lives and works. The significance of that disparity is not lost on him as a Hispanic man serving his community. He described a Hispanic man in his early sixties with no underlying health issues who eventually lost his life to COVID-19 even though the ICU team did everything they could to save him. Ismael was deeply affected “because I’m Hispanic and the majority of the people who have really bad outcomes are part of the Hispanic population.”
New information is released by scientists regularly, offering and examining different risk factors for why some people with the disease only have mild symptoms while others develop a serious illness and even die. This information consistently points to a complex combination of biological and social factors that will take time to fully understand. Ismael and his girlfriend, who is a registered nurse, are passionate about finding answers for the communities they serve. They spend their days off researching. Ismael suspects there is a strong genetic component.
The field of respiratory therapy is changing and there is a lot of demand for RTs, according to Ismael. He says that “if you craft your skillset, there is a place for you.” He also said that some RTs who are close to retirement are getting out early because of the changes in expectations. Medicine is taking a team-centered approach these days, where everyone in the team has input on decision-making, rather than the previous top-down approach where doctors instructed the team on what to do. Now, everyone is expected to collaborate, contribute, and make suggestions. Ismael likes that the field is progressing in that direction because it suits his personality and, more than anything, studies have shown that approach is more effective when it comes to patient care. Whether he is in the ICU treating patients or at home researching COVID-19, that’s what Ismael is all about—what is best for his patients.
Learn More About A Career In Respiratory Therapy
Learn how to become a respiratory therapist, what to look for in respiratory therapy training, and more about this exciting health care career.